Background: Disseminated intravascular coagulation (DIC), an acute or chronic systemic process with multifactorial etiology, can present as a life-threatening emergency with the potential for causing thrombosis and hemorrhage. DIC may be seen with all leukemia subtypes, but it is an especially prominent feature of Acute Myeloid Leukemias (AML). DIC complicating AML can lead to a variety of complications and has been implicated in worse clinical outcome, however, its association with acute cardiovascular complications has not been reported before.
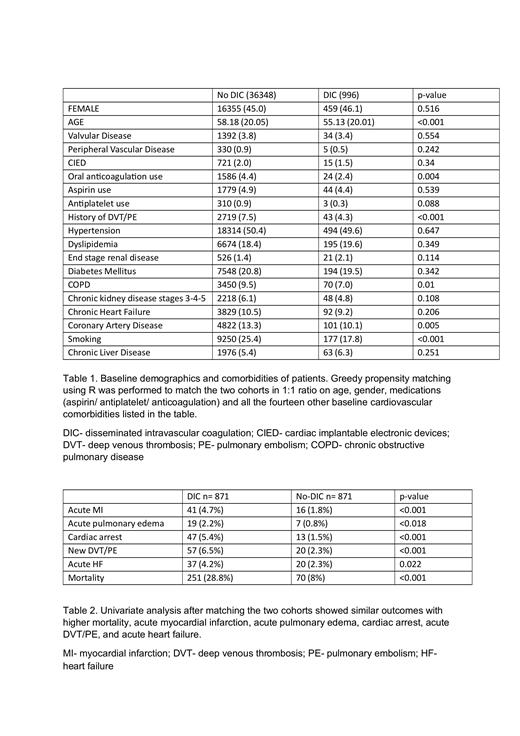
Methods: National Inpatient Sample (NIS) Database 2016 -2018 was used to procure individuals with AML, and baseline demographics and comorbidities were collected using ICD-10-DM codes. Patients with missing data or those receiving immunotherapy, chemotherapy, or radiation during hospitalization were excluded. Patients were stratified into those with and without DIC. Greedy propensity matching using R was performed to match the two cohorts in 1:1 ratio on age, gender, medications (aspirin/ antiplatelet/ anticoagulation) and fourteen other baseline cardiovascular comorbidities. Univariate analysis pre and post-match along with binary logistic regression analysis post-match were used to analyze outcomes. P-value of <0.05 was considered statistically significant.
Results: Out of a total of 37344 patients with AML, 996 had DIC. DIC patients were younger, predominantly males, and had lower prevalence of baseline cardiovascular comorbidities. On pre-match univariate analysis, DIC patients had statistically significant higher mortality (30.2% vs 7.8%), acute myocardial infarction (5.1% vs 1.8%), acute pulmonary edema (2.3% vs 0.7%), cardiac arrest (6.4% vs 0.9%), and acute DVT/PE (6.6% vs 2.7%). Multivariate logistic regression model after matching showed similar outcomes with higher mortality (OR:4.63), acute myocardial infarction (OR:2.64), acute pulmonary edema (OR:2.75), cardiac arrest (OR:3.77), acute DVT/PE (OR:2.98), and acute heart failure becoming statistically significant (OR:1.89) in DIC patients.
Conclusion: DIC was significantly associated with higher mortality and acute cardiovascular complications in patients with AML. The underlying mechanisms involve a complex interplay of procoagulant factors, anticoagulant deficiencies, cytokine release, and endothelial dysfunction. Additionally, leukemic blasts and their interactions with platelets and endothelial cells contribute to microthrombi formation and subsequent organ damage. These findings highlight the importance of close cardiovascular monitoring and prompt recognition of complications in AML patients with DIC. Further studies are needed to corroborate these findings and develop targeted interventions for prevention and management of these complications.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal